A person usually drinks about 2.5 liters of water per day. To this volume should be added another 400 ml, which are formed as a result of the breakdown of fats, carbohydrates and proteins. The main organs that remove water from the body are the kidneys. A small part of it is excreted by the lungs, skin and feces. Many have heard such concepts as primary and secondary urine. But few people know what it is. Often patients turn to the doctor with a request. “Explain where and how primary urine is formed,” they ask. In this article we will cover this issue in more detail.
general information
In the renal nephrons, two phases of fluid formation are observed. It is then transported by the kidneys. Let's try to clearly explain the process of fluid formation in the kidneys. So we will answer a common question that patients ask in the following form: “Explain where and how primary urine is formed.” How do the phases go? Primary urine is formed in nephron bodies. The second phase takes place in the nephron tubules. Primary urine is formed from glomerular capsules, the walls of the capillaries and the inner leaf of which have the property of filtration. Capillary blood in the glomeruli flows under greater pressure than in other organs. 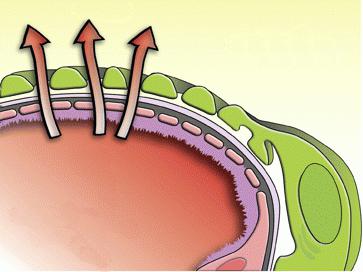 This is created due to the difference in the diameter of the vessels that bring and carry away blood, which is twice as large in the former. High blood pressure promotes its filtration through the walls of the capillaries into the glomerular capsule. Thus, primary urine is formed as a result of a difference in pressure. During the day, the kidneys pass blood through themselves, which comes into contact with the inner walls of the blood vessels. Their area in glomeruli reaches 1.5-2 m². Answering the request of patients: “Explain where and how primary urine is formed,” some numbers should be given. So, about 180 liters of fluid are produced per day, which is then transported from the body. At the same time, one liter of it undergoes filtration with 10 liters of flowing blood.
This is created due to the difference in the diameter of the vessels that bring and carry away blood, which is twice as large in the former. High blood pressure promotes its filtration through the walls of the capillaries into the glomerular capsule. Thus, primary urine is formed as a result of a difference in pressure. During the day, the kidneys pass blood through themselves, which comes into contact with the inner walls of the blood vessels. Their area in glomeruli reaches 1.5-2 m². Answering the request of patients: “Explain where and how primary urine is formed,” some numbers should be given. So, about 180 liters of fluid are produced per day, which is then transported from the body. At the same time, one liter of it undergoes filtration with 10 liters of flowing blood.
Compound
In answer to the request: “Explain where and how primary urine is formed,” it is necessary to say about its composition, since the area of formation of the liquid has a direct impact on its structure. The 1st phase of formation contains almost all blood components. The exception is high molecular weight proteins and formed elements. Primary urine also contains metabolic products such as urea, uric acid and others. Next, it passes from the glomeruli to the nephron tubules, where amino acids, vitamins, glucose, water and salts are reabsorbed into the blood. This process is called reabsorption. In the event that it is in the blood big number individual substances, some of them are not absorbed back. 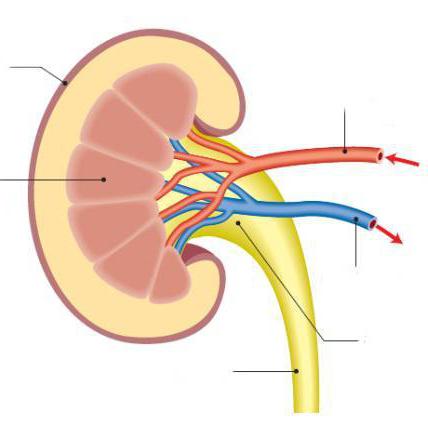
Properties
The main characteristics of primary urine include:
- Low which occurs due to membrane equilibrium.
- Large volume formation per day. It can be tens of liters. Considering that all the blood passes through the kidneys almost three hundred times, during the day this organ is capable of filtering up to one and a half thousand liters of blood. Thus, about 180 liters of urine are produced in the first phase.
From the urine formed in the first phase, substances beneficial to the body are absorbed into the blood.
Glomerular filtration rate (GFR)
GFR is regulated by nervous and humoral mechanisms. influences the following components:
The tone of the glomerular arterioles, affecting the amount of passing blood and the level of filtration pressure;
The tone of mesangial cells, which are connective tissue, located between the capillaries of the nephron glomerulus and the filtration surface;
Vigor of visceral epithelial cells and their functioning.
Some humoral effects, which include prostaglandids, adrenaline, norepinephrine, atriopeptides, adenosine and others, can increase or decrease the glomerular filtration rate. The most important role in its persistence is played by autoregulation of cortical blood flow.
Formation of secondary urine and its composition
During the day, 1.5 liters of this liquid are produced. To form it, 150-180 liters of primary material is required. Through the excretory tract it enters the bladder. From there it is further excreted from the body. About 99% of the water contained in primary urine and the beneficial substances contained in it are absorbed in the tubules. The composition of the secondary liquid differs significantly from that formed in the 1st phase. It does not contain sugar, most salts and amino acids. However, there is increased level concentrations of sulfates, urea, phosphates and other components.
Kidney functions
If there is a lack of table salt in the body, it is not excreted in the urine. This means that the kidneys perform the function of normalizing the level necessary substances contained in the human body. That is, they help remove excess and retain missing components. In the nephron tubules, in addition to the reabsorption of water and substances contained in it, components may enter the urine that are not able to undergo renal filtration on the way from the capillaries to the glomerular capsule. Such elements are medicines (mainly antibiotics), paints and others. Urine that forms in the kidneys passes into the ureters from the renal calyces, passing through the pelvis. Thanks to the rhythmic contractions of the muscles of the transport channels, the liquid enters the bladder. However, urine lingers there for some time before it is filled.
The process of urine formation occurs in the nephrons in two phases: the first phase is the formation of primary urine and the second phase is the formation of secondary, or final, urine.
Primary urine is formed by filtering in the renal corpuscles from the blood flowing through the capillaries of the vascular glomerulus. Through the wall of the glomerular vessels and the inner leaf of the Shumlyansky-Bowman capsule, part of the water and other substances contained in the blood passes into its lumen. In my own way chemical composition primary urine corresponds to blood plasma, but is devoid of proteins. The process of filtration of primary urine in the renal corpuscles is possible due to high blood pressure in the capillaries of the glomerulus. A sharp decrease in blood pressure leads to a decrease in urine output. Usually, not all vascular glomeruli function in the kidneys, but some of them alternately.
Secondary, or final, urine is urine that is excreted from the body to the outside. It is formed from primary urine along the urinary tubules of the nephron by reverse suction into the blood (by reabsorption) of water and some substances dissolved in it that cannot be removed from the body. According to scientists, about 100 liters of primary urine are produced per day, and only about 41.5 liters of secondary urine are released. Primary urine differs in composition from secondary urine: the first, unlike the second, contains glucose, amino acids and some other substances. All these substances, as well as most of the water, when primary urine flows through the nephron tubules, are absorbed back into the blood - into the blood capillaries that weave around the urinary tubules and are branches of the efferent vessels. Substances that must be removed from the body, primarily protein breakdown products, are almost not absorbed back into the blood. The epithelium of the walls of the urinary tubules, in addition to the ability to selectively absorb certain substances from the urinary tubules into the blood, also has a secretory function - it actively releases certain substances from the blood into the urinary tubules (creatine, etc.).
From the nephrons, secondary urine enters the papillary ducts, and from them into the minor calyces. Small calyces (there are 8 - 12 in one kidney) open into 2 - 3 large calyces, the latter into the renal pelvis. From the pelvis, urine passes through the ureter into the bladder.
The most important function of the kidneys is to maintain a constant salt composition of the blood. Various salts and some other substances are excreted from the blood in the urine at different rates depending on the processes occurring in the body. Thus, during gastric digestion, chloride ions from the blood plasma are intensively used by the stomach glands to form hydrochloric acid, and accordingly, the excretion of these ions in the urine decreases. When salts enter the blood excessively, their excretion in the urine increases. Thanks to this, the concentration of salts in the blood plasma is maintained at a constant level. At the same time, a relative constancy of the level of osmotic pressure and a certain chemical balance between acidic and alkaline substances is maintained in all tissues of the body.
Regulation of urine formation. Kidney function is regulated by the nervous system and the humoral pathway. As a result of nervous and humoral influences, contraction or expansion occurs blood vessels kidneys, the permeability of the walls of the vascular glomeruli and the absorption capacity of the epithelial cells of the urinary tubules change. All this affects the process of urine formation. For example, when the blood vessels of the kidneys narrow, the blood flow to them decreases, which leads to a decrease in urine formation. An increase in the permeability of the walls of the vascular glomeruli or a decrease in the absorption capacity of the cells of the urinary tubules is accompanied by an increase in urine formation and even a change in the composition of urine, etc. The significance of the nervous regulation of kidney function is summarized as follows. A large number of sympathetic fibers, as well as fibers from the vagus nerve, approach the kidneys. Irritation of these fibers in animal experiments usually causes a decrease in diuresis. It is also known that severe painful stimulation experienced by humans and animals is accompanied by a decrease or complete cessation (anuria) of urine formation; this phenomenon is associated with excitation of the sympathetic system, which causes contraction of the blood vessels of the kidneys. The process of urine formation is also influenced by special clusters of nerve cells - nuclei located in the diencephalon (in the hypothalamus). These kernels using large quantity nerve fibers connected to the pituitary gland.
Research by K. M. Bykov proved the connection between the cerebral cortex and the kidneys. In his laboratory, experiments were carried out with a conditioned reflex increase in urination. The introduction of water into the animal's body was combined with the action of another stimulus, for example, with the beats of a metronome. At the same time, naturally, urine formation increased due to the introduction of water. After several such combinations, metronome beats alone without introducing water caused increased urine separation, which was the result of the production conditioned reflex. It has also been proven that in the vessels of the kidneys, like other internal organs, there are sensitive nerve endings, the irritation of which reflexively changes the activity of the cardiovascular and respiratory systems.
Of the humoral factors influencing the process of urine formation, highest value have some hormones (see Chapter IX. Endocrine glands). Thus, in the posterior lobe of the pituitary gland there is an antidiuretic hormone, which enhances the reabsorption of water into the blood in the urinary tubules of the nephrons, and thus causes a decrease in the amount of final urine. With a temporary excess of water in the body, the effect of the antidiuretic hormone of the pituitary gland stops and urine formation increases, and, conversely, with a lack of water, this effect of the hormone increases and the amount of urine decreases. At the same time, its concentration increases. Some people experience hypofunction of the posterior lobe of the pituitary gland, which is expressed in a decrease in the release of antidiuretic hormone. In this case, there is a violation of the process of reabsorption in the urinary tubules and the release of large amounts of urine (diabetes insipidus).
The process of urine formation is also influenced by other hormones: the thyroid hormone thyroxine, adrenal hormones - adrenaline, cortisone, etc. Thus, the hormone thyroxine reduces the reabsorption of water in the urinary tubules, which leads to an increase in diuresis. The action of adrenaline is associated with a narrowing of the afferent vessels of the glomeruli. As a result, the pressure in the glomeruli decreases, which leads to a decrease in filtration and also to a decrease in diuresis. Cortisone, in contrast to the antidiuretic hormone of the posterior lobe of the pituitary gland, reduces the reabsorption of water in the renal tubules, resulting in increased diuresis.
Protein breakdown products (urea, etc.) also affect kidney activity, causing increased urine secretion.
The influence of humoral factors on the process of urine formation was proven in experiments with kidney transplantation in animals, when the direct connection of this organ with the nervous system was turned off. In the transplanted kidney, urine output began immediately after the restoration of blood circulation in it.
In conclusion, it should be noted that the influences of nervous and humoral factors on the process of urine formation are interrelated. In particular, nervous system can have such an effect not only directly through the nerve fibers going to the kidneys, but also through the endocrine glands, for example, through the pituitary gland.
Urine
Urine(urina) - straw-yellow liquid, slightly acidic reaction. On average, a person excretes about 1.5 liters of urine per day; its specific gravity is slightly higher than the specific gravity of water (more than one) and is determined by the numbers 1016 - 1020 1.
1 (For comparison, we point out that 1 liter of water weighs 1000 g, and 1 liter of urine weighs 1015 - 1020 g.)
Composition of urine. Urine consists of water and organic substances dissolved in it. In urine healthy person(“normal” urine) contains about 95% water and 5% other substances. Organic matter excreted in the urine are predominantly protein breakdown products. These include urea, uric acid, creatine, hippuric acid and other substances. Most of them contain nitrogen (nitrogen-containing substances). From inorganic substances urine contains table salt, salts of sulfuric and phosphoric acids, potassium oxide, etc.
In total, the daily amount of urine contains about 60 g of organic and inorganic substances. Urea (25 - 30 g) and table salt (10 - 15 g) are excreted in the urine in the greatest quantities. As part of urea, about 9/10 of the total nitrogen contained in protein breakdown products is removed from the body. Thanks to the excretion of table salts and other salts through the kidneys, a constant composition of salts in the blood is maintained.
In addition to the substances listed above, the urine of a healthy person may contain gases (carbon dioxide, etc.), single leukocytes and exfoliated epithelial cells of the urinary tract.
Quantity, composition and properties of urine subject to significant fluctuations depending on various conditions: temperature and humidity environment, the nature of the work, the quantity and composition of food, the amount of water taken, etc. For example, the amount of urine decreases with increased sweating, dry eating, limited water intake, etc. And, conversely, in cold damp weather, when taking liquid food and Large amounts of water increase urination. During the day, urine is usually released more intensely than at night. Simultaneously with the change in the amount of urine, its specific gravity changes. As the amount of urine decreases, the specific gravity usually increases. With increased urine output, it falls. The specific gravity of urine can fluctuate between 1002 and 1030. To determine the specific gravity of urine, a special device is used - a urometer.
The color intensity of the sword can also change. The color depends on the amount of special pigments in the urine (urobilin, urochrome), which are formed from bile pigments. It should be borne in mind that the color of urine can also change due to diseases (jaundice, hemorrhages in the kidneys and urinary tract, etc.) and after taking certain medications.
The reaction of urine is influenced by the composition of food. With long-term use of a plant-based diet, the reaction may not be slightly acidic, as with a varied diet, but alkaline.
All metabolic changes in the body and various kidney dysfunctions are reflected in the composition of urine. Therefore, as a rule, a urine test is performed on each patient. In some diseases, changes in the composition of urine are very characteristic, for example, in the urine of a healthy person there is usually no protein, sugar and blood. They may be present in the urine of patients (“pathological” urine).
The appearance of proteins in the urine is called albuminuria. Prolonged albuminuria is a sign of kidney disease, accompanied by an increase in the permeability of the blood capillaries of this organ. A short-term appearance of protein in the urine can occur during very hard physical work. The appearance of sugar in the urine is called glucosuria. Prolonged glucosuria is a sign of diabetes (diabetes). This disease develops with insufficient secretion of the pancreatic hormone - insulin (see Chapter IX. Endocrine glands). The short-term appearance of sugar in the urine may be due to the intake of large amounts of carbohydrates.
The appearance of blood in the urine is called hematuria. The degree of hematuria varies: from the presence of a small amount of red blood cells, detectable only under a microscope, to the presence of blood, detected by the eye. Hematuria indicates damage to the glomeruli of the kidneys or hemorrhage in the urinary tract.
In pathological urine, one can also find renal epithelial cells stuck together in columns - casts, microbes, a large number of leukocytes, etc.
Sometimes kidney stones form in the urinary tract, usually in the renal pelvis, from salts in the urine. Kidney stones can cause attacks of acute pain in the kidney area (renal colic).
Ureters
Ureter(ureter) is a tube about 30 cm long (see Fig. 76). Upon exiting the hilum of the kidney, the ureter lies on the posterior abdominal wall and descends into the pelvic cavity, where it pierces the wall Bladder and opens with a hole into the cavity of the bladder. The wall of the ureter consists of three membranes: mucous, muscular and connective tissue (adventitia). The mucous membrane is lined with stratified epithelium. The muscular layer consists of a circular and longitudinal layer of smooth muscle tissue. Thanks to its contractions, the ureter makes peristaltic movements.
Bladder
The bladder (vesica urinaria) is a reservoir of urine (Fig. 78). It is located in the pelvic cavity behind the pubic fusion. Between the pubic fusion and bladder there is a layer of loose fiber. Behind the bladder is the rectum in men and the uterus in women.
The bladder is divided into an upper part - the apex, a middle part - the body and a lower part - the bottom. The wall of the bladder consists of three membranes: mucosa with a submucosal layer, muscle and connective tissue. In addition, from above, partially from the sides and from behind, the bladder is covered with a serous membrane - the peritoneum. The mucous membrane of the bladder forms numerous folds; they are absent only in the area of the bottom of the bladder, where there is a smooth triangular-shaped area - the vesical triangle. At the corners of the latter, both ureters open and the urethra emerges. When the bladder fills, the folds of the mucous membrane smooth out.
The muscularis propria consists of three layers of smooth muscle fibers arranged in different directions.
The average capacity of the bladder in an adult is 350 - 500 ml. When the bladder is strongly filled, its apex rises above the upper edge of the pubic fusion and is adjacent to the anterior abdominal wall.
The structure of the urethra is discussed below.
The act of urination
Emptying the bladder (urination) is regulated by the nervous system and is a reflex act. The mucous membrane of the bladder contains the endings of sensory nerves - receptors. Motor nerves approach the muscular layer. When the bladder fills, urine puts pressure on the bladder wall and irritates the receptors. In response to irritation, the muscular lining of the bladder reflexively contracts and the sphincters of the urethra relax, resulting in urine being expelled. This is facilitated by contraction of the abdominal muscles. Urination usually occurs only if the pressure of urine on the walls of the bladder reaches a certain force. The center of the micturition reflex is located in the sacral spinal cord. But this act is also subordinate to the cerebral cortex, evidence of which is the possibility of voluntary retention of urination.
In some diseases of the nervous system and urinary organs, disturbances in the act of urination are observed (involuntary urination, frequent urge to urinate, bedwetting, etc.).
As a result of glomerular filtration, primary urine . Its composition is similar to blood plasma, but does not contain high-molecular proteins and lipids. In 4-5 minutes, all the blood passes through the kidneys. They receive more blood than any organ in the body, even 4-5 times more than the heart and brain. However, a larger amount of it is used not to nourish the kidneys, but to cleanse the blood of toxic products. As a result of glomerular filtration, 70-120 ml of filtrate is formed per minute, and 100-150 liters per day. The efferent arteriole, leaving the capsule, branches again and forms a network of capillaries that intertwine the convoluted nephron channels along almost their entire length.
During the passage of primary urine through the tubules through the epithelial cells of their walls, a significant amount of water and substances needed by the body are returned to the blood. This process is called reabsorption (reverse absorption). It is carried out at the expense of significant energy costs of the body. Some substances (glucose, amino acids) are completely reabsorbed, and mineral salts and water are absorbed from the tubules into the blood in the quantities required by the body. After reabsorption, urine is called secondary, or final.Material from the site
Secondary urine - This is mainly excess water, sodium chloride and urea. Its yellow color is determined by bile pigments, part of which is absorbed in the small intestine, enters the blood, is filtered by the kidneys, but is not reabsorbed. During the day, the human body produces 1.5-2.5 liters of secondary urine. The amount of urine per day changes with changes drinking regime, ambient temperature, excess salt intake.
The secondary urine should not contain glucose, proteins and blood elements.
On this page there is material on the following topics:
Mechanism of primary and secondary urine
Explain the mechanisms of formation of primary and secondary urine
Explain where and how primary urine is formed briefly
Secondary and primary urine message
Formation of primary and secondary urine in animals
Questions about this material:
Not all waste is removed from the body by the kidneys, but the kidneys are the only organs in the body primarily concerned with removing waste materials. All other organs that also act as "waste collectors" are found in other systems: the lungs (remove carbon dioxide, excess heat and water), skin (removes excess heat, water, carbon dioxide, salts and some urea) and gastrointestinal tract (removes solid waste, water, carbon dioxide, salts and excess heat).
More primitive organisms simply excrete waste products constantly, but we have a bladder to store urine until a socially acceptable opportunity presents itself to get rid of it, through the urethra (urinary canal), which is a small tube that runs from the bladder to the outside world.
Kidneys are the main organ excretory system body, they produce urine. The so-called primary urine, or glomerular filtrate, is practically no different in composition from blood plasma, it only lacks proteins. Therefore, nature provided the second stage - reabsorption, or reverse absorption, of substances dissolved in primary urine and the formation of final urine. This process occurs in the kidney tubules and allows up to 98% of the kidney filtrate to be returned to the body. If it were not for reabsorption, our body would dehydrate itself in just 22-25 minutes!
The final urine consists of 96% water and contains: the final products of metabolism (urea, uric acid, pigments, etc.), mineral salts dissolved in it and a certain number of cellular elements of the blood and epithelium of the urinary organs.
First of all, the characteristics of urine can be used to judge the state of the human genitourinary system. In addition, urine examination helps diagnose a number of diseases of internal organs and dysfunction of the endocrine system.
Urine for analysis, unlike blood, is usually collected by the patient himself. There is no need to follow any special diet before taking the test, but you should be moderate in consumption mineral water, sweets and brightly colored foods and do not expose yourself to excessive physical exertion. Women should not have their urine tested during menstruation.
For the study, the entire portion of morning urine is collected after a thorough toilet of the genitals. Women need to use a soap solution for this, followed by washing with clean water.
Urine is collected in a clean, dry container, well washed of detergents and disinfectants, or in a disposable container specially designed for this purpose.
To prevent elements of inflammation in the urethra and external genitalia from entering the sample, you first need to release a small portion of urine and only then collect the required amount in a jar. To conduct a full laboratory test, about 100 ml of urine is needed.
To ensure that the accuracy of the analyzes is not affected by environmental factors, studies should be carried out no later than 2 hours after receiving the material. They will evaluate it in the laboratory general properties urine (color, transparency, smell), its physicochemical qualities (volume, relative density, acidity) and the morphological composition of the resulting sediment.
Chapter 8. General characteristics of urine
The color of urine in healthy people is usually straw yellow. It can change to reddish (due to the presence of hemoglobin) or brown, due to bile pigments (to clarify, just shake the sample: yellow foam will immediately indicate the presence of bile pigments). A milky white tint indicates the presence of droplets of fat, pus or inorganic phosphorus. Very light and slightly colored urine occurs with polyuria.
The smell of urine has no special diagnostic value. Freshly excreted urine is usually odorless. If a patient with diabetes mellitus has ketone bodies in their urine, the urine acquires a characteristic “apple” odor.
Transparency. In healthy people, urine is transparent, because all the components are in solution. If the urine is already cloudy at the time of excretion, this is due to the presence of a large number of cellular elements, salts, bacteria, and fat.
Chapter 9. Physico-chemical characteristics of urine
Amount of urine
The amount of urine excreted per day by a healthy adult (diuresis) ranges from 1000 to 2000 ml - this is approximately 50-80% of the fluid taken during this time. Daily diuresis is influenced not only by the state of the urinary apparatus itself, but also by a number of extrarenal factors.
A condition in which diuresis exceeds 2 liters is called polyuria and is observed with heavy drinking, diabetes mellitus and diabetes insipidus, and in patients with nephrosclerosis.
When less than 500 ml of urine is excreted per day, one speaks of oliguria, which can be caused by acute renal failure, acute diffuse glomerulonephritis and a general deterioration of blood circulation.
Anuria, or the complete absence of urine output, is observed in severe kidney damage, acute renal failure, peritonitis, poisoning, or blockage of the urinary tract by a stone or tumor.
Changes in both the volume and composition of urine can also accompany hypothermia and physical or mental stress.
Relative density of urine
The relative density of urine (specific gravity) is determined by the concentration of substances dissolved in it (protein, glucose, urea, sodium salts, etc.). Morning urine density values equal to or greater than 1.018 indicate normal renal concentration activity and eliminate the need for more specific tests.
Extremely high or low numbers require further evaluation. Most often, low relative density is a consequence of polyuria, and high (with a volume of morning urine of 200 ml or more) – glucosuria.
Urine reaction (pH)
The urine reaction (pH) is determined using indicator test strips. In healthy people, it is 5.00–7.00 and changes significantly with: diabetes mellitus, feverish conditions and a meat diet, which contribute to its acidification. A slightly alkaline urine reaction (more than 7.00) most likely indicates hematuria, resorption of edema, kidney disease, or a strictly vegetarian diet.
Protein in urine
Protein in urine. Found in patients with damage to the kidneys and (or) urinary tract. With a sharp increase in the permeability of the renal filter (nephrotic syndrome), the concentration of protein in the urine increases (this is called proteinuria) and can reach 100 g/l.
In a healthy person, the concentration of protein in the urine does not exceed 0.002 g/l - such amounts are not detected in single portions of urine by the methods that are currently used.
As a rule, the degree of kidney pathology directly affects the degree of proteinuria: the higher the protein concentration in the urine, the further the pathological process has progressed and the less favorable the prognosis will be. To clarify the degree of proteinuria, they resort to examining 24-hour urine, i.e., material collected by the patient during the day. Based on the amount of protein in daily urine, three degrees of proenuria are distinguished:
Weakly expressed – 0.1–0.3 g/day;
Moderate – less than 1 g/day;
Pronounced – 1–3 g/day or more.
For patients with diabetes mellitus, a “border zone” of proteinuria has been identified - the so-called microalbuminuria. Due to specific kidney damage in diabetes, the appearance of microalbumin in the urine is considered a sign of a reversible stage of the pathology, which can still be eliminated through drug therapy. Therefore, for diabetics, the upper limit of normal protein concentration in urine is considered to be 0.0002 g/l (20 μg/l) and 0.0003 g/day. (30 mcg/day).
Glucose in urine
Glucose in urine. Just like protein, it is not detected by conventional testing methods in the urine of healthy people. It is detected only when consuming excess amounts of carbohydrates in food, psycho-emotional stress, or under the influence of certain medications. In all these cases, the concentration of glucose in the blood exceeds the so-called renal threshold (9.99 mmol/l).
The appearance of glucose in the urine - glucosuria - signals a disruption in the functioning of a number of endocrine organs: for example, the insular apparatus of the pancreas (diabetes mellitus) or the thyroid gland (Graves' disease).
If glucose is detected in the urine, the patient must be sent for further examination on suspicion of diabetes mellitus and the first step is to determine the level of glucose in the blood. Depending on which laboratory examined the patient’s urine, the data obtained can be expressed in mmol/l or in%. To recalculate these values, you can use the following formulas:
Glucose in urine (%) = (glucose in urine (mmol/l) ? 18): 1000;
Glucose in urine (mmol/l) = (glucose in urine (%): 18) ? 1000.
More accurate data can be obtained by determining the daily loss of glucose in urine. This may be necessary to assess the effectiveness of the treatment.
Ketone bodies
Ketone bodies are most often present in the urine in cases of severe diabetes mellitus, sometimes in cases of traumatic brain injury, cerebral hemorrhage, as well as a low-carbohydrate diet and fasting.
In diabetes, a sharp increase in the concentration of ketone bodies can result in ketoacidotic coma - one of the most dangerous complications of this pathology.
Typically, the result of determining ketone bodies in urine is expressed semi-quantitatively: weakly positive reaction (+); positive reaction (+ +) and (+ + +); sharply positive – (+ + + +).
Bilirubin. It is not found in the urine of practically healthy people, but appears in cases of obstructive jaundice and inflammatory processes in the liver.
Urobilin. Freshly released urine contains urobilinogen, which turns into urobilin when standing. In a healthy person, urobilin is contained in the urine in trace amounts, and no more than 6 mg is excreted per day (in children - 2 mg).
Collectively, these bodies are called urobilinoids and are derivatives of bilirubin, excreted in bile and subjected to the action of enzymes of intestinal cells and bacteria living in the intestine.
Detection of urobilin in quantities exceeding the norm is important in the diagnosis of liver diseases and involves clarifying the diagnosis through biochemical, immunological and other tests. Urobilinuria can range from weakly positive (+) to strongly positive (+ + +) and is detected when:
Acute and chronic inflammatory processes in the liver;
Severe hemolysis - massive destruction of red blood cells in the blood during hemolytic anemia.
Chapter 10. Morphological study of urine sediment
A morphological study of urine sediment from a healthy person reveals single erythrocytes, 0–2 leukocytes, 0–3 epithelial cells and up to 50,000 bacteria per 1 ml of urine in the field of view of a microscope. There are no cylinders. In 1 ml of daily urine, examined using the Nechiporenko method, up to 4000 leukocytes, up to 1000 erythrocytes, 0–1 cylinder are normally found.
An increase in the number of leukocytes (leukocyturia) indicates an infectious and inflammatory process in the kidneys and urinary tract. If the number of leukocytes in the field of view exceeds 60, they speak of pyuria.
An excess of red blood cells and the appearance of hemoglobin in the urine is called hematuria and is observed during inflammatory processes in the kidneys and genitourinary tract, with the development of a tumor in the kidneys, and with urolithiasis. Hematuria can be of two types:
When the presence of blood can be determined visually, the urine is more or less colored red and does not require microscopy, since red blood cells will cover the entire field of view. This condition is called gross hematuria;
When the admixture of blood is not visible to the naked eye, but is detected by microscopy. This condition is called microhematuria.
The casts consist of protein, which is deposited on the walls of the renal tubules under the influence of acidic urine. Thus, the appearance of cylinders in the urine sediment can be considered a reliable sign of the appearance of protein in the urine. However, it should be borne in mind that with an alkaline urine reaction, proteinuria does not necessarily lead to the formation of casts.
Determining the types of casts and the inclusions they contain makes it possible to distinguish primary kidney damage from diseases of the lower genitourinary tract.
Most often, hyaline casts are found in urine sediment, signaling kidney pathologies. However, they can also be found in the urine of a healthy person who has been exposed to severe cold or overheating, prolonged standing in an upright position, or heavy physical activity.
Casts with the inclusion of red blood cells with a high degree of certainty indicate acute diffuse glomerulonephritis. Damage to the renal tubules leads to the formation of epithelial casts. Cylinders containing leukocytes and bacteria indicate inflammatory kidney damage. Waxy casts forming in the distal nephron are a sign of severe kidney damage. Fat casts (with small droplets of fat) are present in all forms of nephritis and nephrotic syndrome.
Epithelial cells line the mucous membrane of the urinary tract and are released in large quantities into the urine during inflammation. Since each part of the urinary tract is characterized by its own type of epithelium, the type of epithelial cells in the urine sediment can determine the area suffering from inflammation.
Bacteria in urine is not always a sign of inflammation. Their increased number is of primary importance for diagnosis.
Chapter 11. Tests characterizing renal function
To clarify the diagnosis and determine the severity of kidney damage, doctors often resort to additional tests. Most often these are the Zimnitsky test and the Reberg-Tareev test.
Zimnitsky test
The Zimnitsky test gives an idea of the concentrating function of the kidneys by determining the density of urine collected every 3 hours during the day. Thus, a total of 8 samples are examined.
To conduct the Zimnitsky test, the patient follows his usual drinking regimen and, whenever possible, refuses to take diuretics. The total amount of urine excreted in relation to the liquid drunk is also taken into account.
Rehberg's test
The Rehberg test characterizes the excretory function of the kidneys and the ability of the renal tubules to secrete and reabsorb certain substances.
For the Rehberg test, blood is collected from the patient for one hour, in the morning on an empty stomach. In the middle of this hour, blood is also taken from a vein to determine the creatinine content. Then, using a special formula, the doctor calculates the value of glomerular filtration (GF) and tubular reabsorption.
Normally, EF is 130-140 ml/min. It decreases with nephritis, hypertension and diabetes.
Tubular reabsorption normally falls within the range of 95-99%, but may decrease in healthy people due to heavy drinking or under the influence of diuretics. A pronounced decrease in reabsorption is considered a sign of a primary or secondary wrinkled kidney.
Page 3 of 5
9.3. Urine formation
The kidneys consume 9% of the total amount of oxygen used by the body. The high intensity of metabolism in the kidneys is due to the high energy intensity of the processes of urine formation.
The process of formation and excretion of urine is called diuresis; it occurs in three phases: filtration, reabsorption and secretion.
Blood enters the vascular glomerulus of the renal corpuscle from the afferent arteriole. The hydrostatic blood pressure in the glomerulus is quite high - up to 70 mm Hg. Art. In the lumen of the Shumlyansky-Bowman capsule it reaches only 30 mm Hg. Art. The inner wall of the Shumlyansky-Bowman capsule tightly fuses with the capillaries of the vascular glomerulus, thereby forming a kind of membrane between the lumen of the capillary and the capsule. At the same time, small spaces remain between the cells that form it. A semblance of a tiny lattice (sieve) appears. In this case, arterial blood flows through the capillaries of the glomerulus quite slowly, which maximizes the transfer of its components into the lumen of the capsule.
The combination of increased hydrostatic pressure in the capillaries and low pressure in the lumen of the Shumlyansky-Bowman capsule, slow blood flow and the structural features of the walls of the capsule and glomerulus create favorable conditions for the filtration of blood plasma - the transition of the liquid part of the blood into the lumen of the capsule due to the pressure difference. The resulting filtrate is collected in the lumen of the Shumlyansky-Bowman capsule and is called primary urine. It should be noted that a decrease in blood pressure below 50 mm Hg. Art. (for example, with blood loss) leads to the cessation of the formation of primary urine.
Primary urine differs from blood plasma only in the absence of protein molecules in it, which, due to their size, cannot pass through the capillary wall into the capsule. It also contains metabolic products (urea, uric acid, etc.) and other components of plasma, including substances necessary for the body (amino acids, glucose, vitamins, salts, etc.).
The main quantitative characteristic of the filtration process is the glomerular filtration rate (GFR) - the amount of primary urine formed per unit of time. Normal glomerular filtration rate is 90-140 ml per minute. 130-200 liters of primary urine are produced per day (this is approximately 4 times the total amount of fluid in the body). In clinical practice, the Rehberg test is used to calculate GFR. Its essence is to calculate creatinine clearance. Clearance is the volume of blood plasma, which, passing through the kidneys in a certain time (1 min), is completely cleared of a particular substance. Creatinine is an endogenous substance, the concentration of which in the blood plasma is not subject to sharp fluctuations. This substance is excreted only by the kidneys by filtration. It is practically not subject to secretion and reabsorption.
Primary urine from the capsule enters the nephron tubules, where reabsorption occurs. Tubular reabsorption is the process of transporting substances from primary urine into the blood. It occurs due to the work of cells lining the walls of the convoluted and straight nephron tubules. The latter actively absorb glucose, amino acids, vitamins, Na+, K+, C1 -, HCO 3 - ions, etc. from the nephron lumen into the secondary capillary network of the kidney. For most of these substances, there are special carrier proteins on the membrane of tubular epithelial cells. These proteins, using the energy of ATP, transfer the corresponding molecules from the lumen of the tubules into the cytoplasm of the cells. From here they enter the capillaries that intertwine the tubules. Water absorption occurs passively, along an osmotic pressure gradient. It depends primarily on the reabsorption of sodium and chlorine ions. A small amount of protein that enters the primary urine during filtration is reabsorbed by pinocytosis.
Thus, reabsorption can occur passively, according to the principle of diffusion and osmosis, and actively, due to the activity of the epithelium of the renal tubules with the participation of enzyme systems with energy consumption. Normally, about 99% of the primary urine volume is reabsorbed.
Many substances, when their concentration in the blood increases, cease to be fully reabsorbed. These include, for example, glucose. If its concentration in the blood exceeds 10 mmol/l (for example, with diabetes), glucose begins to appear in the urine. This is due to the fact that carrier proteins cannot cope with the increased amount of glucose coming from the blood into the primary urine.
In addition to reabsorption, the process of secretion occurs in the tubules. It involves the active transport of certain substances from the blood into the lumen of the tubule by epithelial cells. As a rule, secretion occurs against the concentration gradient of the substance and requires the expenditure of ATP energy. In this way, many xenobiotics (dyes, antibiotics and other drugs), organic acids and bases, ammonia, and ions (K+, H+) can be removed from the body. It should be emphasized that each substance has its own strictly defined mechanisms of excretion by the kidneys. Some of them are excreted only by filtration, and are practically not secreted (creatinine); others, on the contrary, are removed primarily by secretion; Some are characterized by both mechanisms of excretion from the body.
Due to the processes of reabsorption and secretion, secondary, or final urine, is formed from primary urine, which is excreted from the body. The formation of final urine occurs as the filtrate passes through the nephron tubules. Thus, from 130-200 liters of primary urine, only about 1.0-1.5 liters of secondary urine are formed and excreted from the body within 1 day.
Composition and properties of secondary urine. Secondary urine is a clear, light yellow liquid containing 95% water and 5% dry matter. The latter is represented by products of nitrogen metabolism (urea, uric acid, creatinine), potassium and sodium salts, etc.
The urine reaction is inconsistent. During muscle work, acids accumulate in the blood. They are excreted by the kidneys and hence the urine reaction becomes acidic. The same thing is observed when eating protein foods. When eating plant foods, the urine reaction is neutral or even alkaline. At the same time, most often urine is a slightly acidic environment (pH 5.0-7.0). Normally, urine contains pigments, such as urobilin. They give it a characteristic yellowish color. Urine pigments are formed in the intestines and kidneys from bilirubin. The appearance of unchanged bilirubin in the urine is characteristic of diseases of the liver and biliary tract.
The relative density of urine is proportional to the concentration of substances dissolved in it ( organic compounds and electrolytes) and reflects the concentration ability of the kidneys. On average, its specific gravity is 1.012-1.025 g/cm3. It decreases with drinking large amounts of liquid. The relative density of urine is determined using a urometer.
Normally, there is no protein in urine. Its appearance there is called proteinuria. This condition indicates kidney disease. It should be noted that protein can also be found in the urine of healthy people after heavy physical activity.
In a healthy person, glucose is usually not found in the urine. Its appearance is associated with an excessive concentration of the substance in the blood (for example, in diabetes mellitus). The appearance of glucose in the urine is called glucosuria. Physiological glucosuria is observed during stress and consumption of increased amounts of carbohydrates.
After centrifuging the urine, the supernatant is obtained, which is used for examination under a microscope. In this case, a number of cellular and non-cellular elements can be identified. The former include epithelial cells, leukocytes and erythrocytes. Normally, the content of epithelial cells of the tubules of the kidneys and urinary tract should not exceed 0-3 in the field of view. This is the normal level of leukocytes. When the content of leukocytes increases above 5 - 6 in the field of view, they speak of leukocyturia; above 60 - pyuria. Leukocyturia and pyuria are signs of inflammatory diseases of the kidneys or urinary tract. Normally, red blood cells in the urine are found in single quantities. If their content increases, they speak of hematuria. Noncellular elements include cylinders and unorganized sediment. Cylinders are protein formations that are not found in the urine of a healthy person. They are formed in the nephron tubules and have a cylindrical shape, repeating the shape of the tubules. Disorganized sediment consists of salts and crystalline formations found in normal and pathological urine. Bacteria can also be found in the urine (the normal value is no more than 50,000 in 1 ml; with large numbers they speak of bacteriuria).
Regulation of urine formation. The amount of urine produced and its composition are variable and depend on the time of day, external temperature, the amount of water drunk and the composition of food, on the level of sweating, muscle work and other conditions.
Urine formation depends primarily on the level of blood pressure. It is also influenced by the degree of blood supply to the kidneys, and, consequently, by the size of the lumen of the blood vessels of these organs. The narrowing of the kidney capillaries and the fall in blood pressure are reduced, and the dilation of the capillaries and the increase in blood pressure increase urine output.
The intensity of urine formation fluctuates throughout the day: during the day it is 3-4 times more than at night. Urine produced at night is darker and more concentrated than urine produced during the day. With prolonged physical activity, urination decreases due to increased sweating - most The body releases fluids through evaporation. The same thing happens when the external temperature increases: on hot days, the amount of urine decreases and it becomes more concentrated. Drinking large amounts of water increases diuresis. Short-term and intense muscle work also increases urine formation, which depends mainly on the increase in blood pressure during exercise.
The autonomic nervous system plays an important role in regulating kidney function. Under the influence of the sympathetic nervous system, vasoconstriction of the kidneys occurs, and accordingly, the glomerular filtration rate decreases. In addition, sympathetic impulses stimulate the reabsorption of sodium and water, thereby reducing diuresis. The parasympathetic nervous system has the opposite, but less pronounced effect on urine formation.
Antidiuretic hormone (vasopressin - a hormone of the posterior lobe of the pituitary gland) increases the reabsorption of water in the renal tubules and reduces diuresis. Under the influence of the adrenal cortex hormone, aldosterone, the reabsorption of Na+ ions and water increases, and the secretion of K+ increases. Adrenaline is a hormone of the adrenal medulla that causes a decrease in urine formation.
If the amount of urine produced during the day increases, we speak of polyuria. A decrease in urine production of less than 500-600 ml/day is called oliguria. A complete cessation of urine output is called anuria.
